Lifestyle medicine is a globally recognised medical discipline with a strong evidence base and widespread practice. The British Society of Lifestyle Medicine (BSLM) is the largest UK medical charity promoting education and awareness within this field.
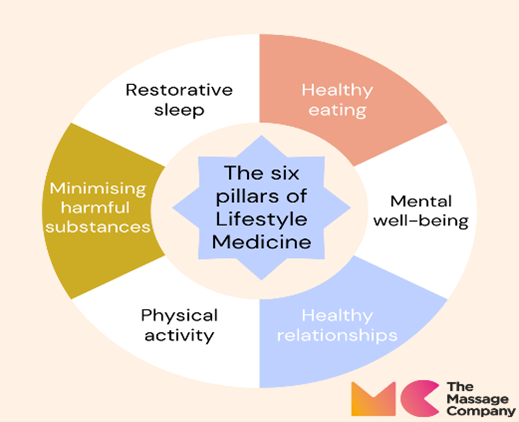
The BSLM defines Lifestyle Medicine as; “Evidence-based, clinical care that supports behaviour change through person-centred techniques to address the 6 pillars of Lifestyle Medicine: (a) healthy eating, (b) mental wellbeing, (c) healthy relationships, (d) physical activity, (e) minimising harmful substances and (f) restorative sleep.”
Lifestyle medicine describes the work that clinicians from all backgrounds can do to support their patients with lifestyle changes.
Lifestyle Medicine operates from a holistic health approach that works to treat root causes of health issues. Lifestyle medicine uses evidence-based methods to uncover the cause of illnesses or chronic conditions by treating or preventing associated symptoms. For example, working to relieve stress to combat tension headaches, digestive issues or insomnia would be a lifestyle medicine practice.
Practicing in lifestyle medicine is proposed in response to the current public health emergency in lifestyle-related non-communicable diseases (Hay et al., 2017). The NHS long term plan (NHS, 2019) signals a shift towards preventative medicine, in which lifestyle medicine has a central role.
How Does Lifestyle Medicine Work?
Lifestyle Medicine is based upon the idea that the body can heal itself. It focuses on treating the entire physical and mental systems to improve function and well-being, through lifestyle intervention.
Choosing to pursue treatment through lifestyle medicine doesn’t mean that one rejects all conventional medicine. Lifestyle Medicine treatment can work in conjunction with other conventional or western medicine treatments. A lifestyle medicine practitioner guides the patient on a path to fostering healthier habits. It is based on the idea that the body can’t begin to heal itself until it has a base level of health.
A therapist or healthcare provider that uses lifestyle medicine within their role should understand how to assess and support improvements within the six pillars of lifestyle medicine:
TMC facts
In our Camberley Centre, between January and December 2024;
• 77% of our customers came to see us with muscular pain
• 59% of our customers came to see us with stress related symptoms
• 11% of our customers came to see us with sleep difficulty
Massage and lifestyle medicine
There are cultural shifts happening that give massage therapy an advantage in health care environments, the primary one being the distinct movement away from what Dr. Brent Bauer, director of the Complementary and Integrative Medicine Program at the Mayo Clinic, describes as “fixing what’s broken” toward preventive medicine. Massage therapy has played an integral and important role in this setting by helping patients take better care of themselves and live with less stress and pain.
There is evidence that supports the benefits of massage therapy for sleep quality and mental well-being, such improvements could assist in more positive, healthier relationships. A meta-analysis found that people with serious mental illness often cited improving their health, mood, and reducing stress as reasons for exercising. However, low mood and stress were also common barriers to exercise (Firth et al., 2016). Pain and stress reduction achieved through massage could encourage increased exercise levels. Pain is associated with increased drug and alcohol consumption. Smokers with greater pain severity may also report hazardous patterns of alcohol use. Reduced pain levels are likely to reduce reliance on harmful substances (LaRowe et al., 2020).
References
https://bslm.org.uk/core-accreditation/
https://www.amtamassage.org/publications/massage-therapy-journal/massage-therapy-and-integrative-medicine/
https://www.nhs.uk/live-well/
LaRowe, L. R., Powers, J. M., Paladino, M. B., & Ditre, J. W. (2020). Pain Severity and Alcohol Use Among Daily Tobacco Cigarette Smokers. The American journal on addictions, 29(2), 134–140. https://doi.org/10.1111/ajad.13003